Mental health care can be expensive, and the cost of therapy sessions can add up fast. Luckily, if you’re covered by Ohio Medicaid, your mental health care may be covered. This article helps you understand what’s covered, what’s not, and how to use your Ohio Medicaid coverage for mental health care.
Key takeaways
- Ohio Medicaid covers online and in-person therapy and mental health care services like individual therapy, family therapy, group therapy, and high-intensity services for severe conditions.
- Eligibility for Ohio Medicaid is based on income, residency, and specific health needs. Special programs, like EPSDT for children, offer expanded benefits.
- Costs for therapy are generally low to none for most Ohio Medicaid recipients. Small copays may apply in limited situations.
- Therapy services must be deemed medically necessary in order to fall under Ohio Medicaid coverage.
- Finding an in-network therapist is straightforward through Ohio Medicaid’s provider portal, customer service, or platforms like Grow Therapy.
Introduction to Ohio Medicaid
Ohio Medicaid provides essential health benefits to low-income residents across the state, including families, seniors, and individuals with disabilities. The program covers a broad range of services, including medical, dental, and behavioral health care, ensuring qualified Ohioans can access necessary health support.
Mental health care under Ohio Medicaid includes coverage for various types of therapy, such as individual counseling, family therapy, and group therapy. Common treatment options such as cognitive behavioral therapy (CBT) and medication management are covered. Additionally, Ohio Medicaid supports substance use treatment and high-intensity services such as crisis intervention.
Who is eligible for Ohio Medicaid?
Eligibility for Ohio Medicaid is based on several factors including income, residency, and specific health needs. Ohio residents with low incomes who meet financial requirements, are U.S. citizens, or meet Medicaid non-citizen requirements, and hold or can obtain a social security number may qualify for coverage.
Special coverage options are available for specific groups. Children up to age 21 can receive expanded services through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program, which ensures access to preventive and developmental care. Pregnant women and individuals with disabilities are also eligible for enhanced benefits that address their unique health needs.
Determining medical necessity
For therapy and mental health services to be covered, they must be deemed “medically necessary” by a provider. Under Ohio Medicaid rules, conditions of medical necessity for a service are as follows:
- It meets generally accepted standards of medical practice
- It is clinically appropriate in its type, frequency, extent, duration, and delivery setting
- It is appropriate to the adverse health condition for which it is provided and is expected to produce the desired outcome
- It is the lowest cost alternative that effectively addresses and treats the medical problem
- It provides unique, essential, and appropriate information if it is used for diagnostic purposes
- It is not provided primarily for the economic benefit of the provider, nor for the sole convenience of the provider or anyone else other than the recipient.
Providers assess the medical necessity of therapy services based on the individual’s health needs, ensuring that coverage is available for treatment that will make a meaningful difference in the person’s mental and physical well-being.
Does Ohio Medicaid cover therapy?
Yes, Ohio Medicaid typically covers therapy — including in-person and online therapy — as well as a wide range of mental health services that are designed to help with substance abuse, depression, anxiety, stress, relationship issues, and more.
What therapy does Ohio Medicaid cover?
Ohio Medicaid insurance covers many types of therapy that serves as quality care options for a variety of conditions. You will need to confirm what types of therapy your specific Ohio Medicaid plan covers, but in general, Ohio Medicaid typically covers:
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Therapy for attention-deficit/hyperactivity disorder (ADHD)
- High-intensity services for those with severe and persistent mental illness
- Medication-assisted treatment (MAT)
- Peer support services
- Family therapy
- Group therapy
Ohio Medicaid covers mental health treatment and behavioral health services from the following types of providers:
- Community behavioral health agencies
- Licensed Marriage and Family Therapists (LMFT)
- Licensed Clinical Social Workers (LCSW)
- Psychologists
- Psychiatrists
- Hospitals
- Residential facilities
- Peer support specialists
Learn more about other types of therapy you might find when seeking mental health care. Be sure to double check your specific Ohio Medicaid health plan, or reach out to Ohio Medicaid directly, to understand what therapy may be covered by your Ohio Medicaid insurance.
Search for therapists who accept Ohio Medicaid
Medication coverage with Ohio Medicaid
Ohio Medicaid provides coverage for a range of medications to support the treatment of mental health conditions, such as depression, anxiety, bipolar disorder, and schizophrenia. Commonly covered medications include antidepressants, antipsychotics, mood stabilizers, anti-anxiety drugs, and medications for ADHD. These medications help Medicaid recipients manage symptoms and improve mental health outcomes. For individuals enrolled in the MyCare Ohio program, medication coverage is included as part of comprehensive care coordination, which integrates physical, behavioral, and long-term care services for dual-eligible members.
For high-cost or specialized medications, such as certain long-acting injectables or newer treatments, Ohio Medicaid may require prior authorization. This process ensures that the medication is deemed “medically necessary” by a healthcare provider, who must submit documentation to justify its use.
Medicaid also provides coverage for medications involved in opioid treatment programs, supporting recovery, and symptom management for those with substance use disorders. Inpatient settings may also provide these medications when appropriate, with Ohio Medicaid’s coordinated care approach ensuring a seamless transition from inpatient to outpatient care.
What types of therapy does Ohio Medicaid not cover?
Ohio Medicaid covers many types of therapy which may help an individual with their mental health needs. However, there are some types of mental health services which are not covered by Ohio Medicaid. These services include, but may not be limited to:
- Hypnotherapy: Hypnotherapy uses hypnosis to help people with their mental health problems. Although some people find it helpful, Ohio Medicaid does not believe it is a reliable or effective treatment for mental health issues.
- Non-traditional therapy: Non-traditional therapy, such as biofeedback therapy, aims to help people control their body’s response to stress and anxiety by giving them feedback about their body’s functions, like their heart rate or blood pressure. Ohio Medicaid does not cover this type of therapy because they do not think there is enough evidence to prove that it’s an effective form of treatment.
Does Ohio Medicaid cover online therapy?
Yes, Ohio Medicaid covers both online therapy (also known as telehealth or virtual therapy) in addition to traditional in-person therapy. This option allows Medicaid recipients to access mental health services remotely, which can be particularly helpful for individuals in rural areas, those with limited transportation options, or those with mobility challenges. It’s important to check with your specific provider to see if they offer online therapy.
Does Ohio Medicaid cover out-of-network therapy?
Ohio Medicaid covers out-of-network therapy in unique and uncommon circumstances. If you want to see an out-of-network mental healthcare provider with Ohio Medicaid, it may cost much more than seeing an in-network provider. You may have to pay out of pocket, and you should check beforehand to see if you will be able to file for any kind of reimbursement from Ohio Medicaid. If you have questions about out-of-network therapy coverage, please refer to your Ohio Medicaid summary of benefits (SOB) as described below, or contact Ohio Medicaid directly.
How to check if your Ohio Medicaid plan covers therapy
There are two main ways to find out if your Ohio Medicaid plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your Ohio Medicaid “summary of benefits”
On the summary of benefits (SOB), look for a row that references mental health, behavioral health, or substance abuse services, as well as “outpatient services” (because therapy is considered to be outpatient care).
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your Ohio Medicaid plan does cover mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered”, then your Ohio Medicaid plan does not cover mental health services such as therapy.
To learn more about how Summary of Benefits are structured, you can refer to this sample SOB from the Centers of Medicare & Medicaid Services website.
2. Contact Ohio Medicaid directly
Contacting Ohio Medicaid directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for Ohio Medicaid, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the Ohio Medicaid website to log into your account, and either chat or email a Ohio Medicaid representative directly
How much does Ohio Medicaid therapy cost?
For most people, the typical cost for therapy under Ohio Medicaid is low to none, as copayments are generally not required for standard mental health services. In some cases, a small copay of $3 may apply for specific services, such as non-emergency visits to a hospital emergency room.
However, individual costs may vary based on the managed care plan’s network requirements and any additional services required. If you are insured by Ohio Medicaid, it’s best to confirm your exact out-of-pocket costs with your plan or provider before your appointment to avoid any unexpected fees.
Ohio Medicaid therapy copay
When paying for therapy, your copay (or copayment) is an important potential cost you should know about.
A copay is a fixed amount you may have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double-check for a potential copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to Ohio Medicaid support directly.
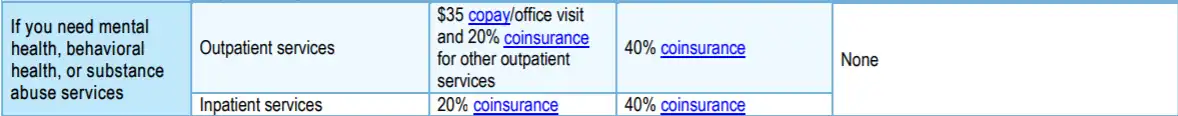
Example Only
What do terms like deductible, copay, and coinsurance mean?
Navigating the insurance system — especially when you’re in need of mental health support — can be challenging and confusing. For help, please visit our Understanding health insurance article.
Does Ohio Medicaid require a referral to see a therapist?
Generally, you do not need a referral from your primary care provider to access mental health care services under Ohio Medicaid. However, some treatments and services may require prior authorization. Consult your specific Medicaid plan or contact Ohio Medicaid directly to understand the requirements and ensure you receive the necessary care.
How to find a therapist covered by Ohio Medicaid
Finding a therapist who accepts Ohio Medicaid insurance is not as difficult as you might think.
1. Ohio Medicaid directory of therapists
Ohio Medicaid offers an online provider portal where you can search for a mental health professional. You can filter by location, specialization, and more.
Using Ohio Medicaid’s online directory can save you time and effort in finding a mental health provider. Instead of calling multiple providers to see if they accept your insurance, you can quickly and easily find in-network providers in your area with just a few clicks.
2. Contact Ohio Medicaid customer service
To locate a mental health professional covered by Ohio Medicaid, you can contact Ohio Medicaid Customer Service for assistance. The customer service team can provide you with information about in-network providers, explain coverage details, and guide you through the process of finding a therapist who accepts Ohio Medicaid.
How to Contact Ohio Medicaid Customer Service:
-
- Phone: Call the Ohio Medicaid Consumer Hotline at 1-800-324-8680 for direct assistance. Representatives are available to answer your questions and help locate providers.
- Hours of operation: Customer service is available Monday through Friday from 7:00 a.m. to 8:00 p.m., and on Saturdays from 8:00 a.m. to 5:00 p.m.
- Online: Fill out the contact form (Do not add personal information beyond what the form requests).
3. Use a therapy provider like Grow Therapy
With Grow Therapy, you can search for licensed mental health providers who are in-network with Ohio Medicaid and provide both in-person and online therapy. At this time, Grow Therapy works with providers who accept Buckeye Health Plan Managed Medicaid, Buckeye Health Plan Medicaid, MyCare Ohio Medicare-Medicaid, Humana Dual Medicare & Medicaid, and UnitedHealthcare/Optoum Medicaid.
On Grow Therapy, you can browse our growing network of vetted therapists and use filters to search by age, specialty, gender, and more. Simply pick the therapist who meets your unique needs and book your first session.
When booking, you’ll be asked to enter your insurance information to verify eligibility and receive a cost estimate.
Navigating common issues with Ohio Medicaid mental health coverage
Navigating Ohio Medicaid’s mental health coverage can sometimes present challenges. Here’s a step-by-step guide to troubleshooting common issues, including denied claims and pre-authorization requirements, and how to address them effectively.
Denied claims
A claim denial can occur if a service doesn’t meet Medicaid’s criteria for coverage, if there’s missing documentation, or if the provider isn’t in-network.
What to try: First, review the explanation of benefits (EOB) or denial notice to understand the reason for the denial. Contact your Medicaid Managed Care Plan’s (MCP) customer service department to ask for clarification. Gather any additional documentation that may support your claim, such as treatment notes or a provider’s statement of medical necessity, and file an appeal within the specified time frame (typically 90 days from the denial date). For help with the appeal process, call the Ohio Medicaid Consumer Hotline at 1-800-324-8680.
Needing pre-authorization
Some mental health services, especially high-cost treatments or specialized therapies, may require prior authorization to ensure they are “medically necessary” for the patient.
What to try: If your provider recommends a service that requires prior authorization, ask them to submit the necessary forms to your managed care plan before your appointment. This will help prevent delays or unexpected costs. Make sure to follow up with both your provider and Medicaid plan to confirm approval before receiving the service. If the pre-authorization request is denied, you can file an appeal or request a State Fair Hearing.
Other issues and solutions
- Out-of-network services: If you need a mental health provider who isn’t in-network, contact your Medicaid plan to discuss options. In some cases, if the service is unavailable in-network, your plan may approve out-of-network coverage. Obtain authorization beforehand to avoid out-of-pocket costs.
- Billing errors: Sometimes, you may receive a bill for a service that should have been covered by Medicaid. Contact your provider’s billing department to ensure they billed the service correctly under Medicaid. You can also contact your MCP to verify coverage and assist with resolving the issue.
- Understanding copays and costs: Ohio Medicaid typically covers mental health services at no cost to most beneficiaries. If you’re charged a copay or fee, verify whether you fall into an exempt group (such as individuals under 21 or pregnant women). If you believe you’ve been wrongfully charged, contact Ohio Medicaid customer service or request a state hearing.
By understanding these common issues and knowing how to navigate them, you can make the most of your Ohio Medicaid mental health coverage. For additional support, contact the Ohio Medicaid Consumer Hotline at 1-800-324-8680 or visit the Ohio Medicaid website.
Making the most of your mental health coverage with Ohio Medicaid
Ohio Medicaid offers valuable mental health resources if you know how to make the most of your coverage. Regularly checking your plan details keeps you informed of any changes and helps avoid unexpected costs.
Being proactive is key — seek support as soon as you notice symptoms. Ohio Medicaid covers a range of mental health services, from individual counseling to more intensive care. If challenges arise, like denied claims or needing authorization, don’t hesitate to reach out to customer service for help.

