Mental health care can be costly, and therapy expenses can add up quickly. If you’re covered by Texas Medicaid, you may be eligible for comprehensive mental health benefits to help manage these costs.
This guide will walk you through what’s covered, what isn’t, and how to make the most of your Texas Medicaid plan for mental health care. Understanding your coverage ensures you can access the services you need while minimizing out-of-pocket expenses.
Key takeaways
- Texas Medicaid provides a variety of mental health services, including individual, family, and group therapy, as well as medication management.
- Coverage is available for eligible low-income individuals, including children, pregnant women, people with disabilities, and seniors.
- Therapy costs under Texas Medicaid are minimal, with many services fully covered or requiring small copays.
- Telehealth is covered under Texas Medicaid, improving accessibility for those in rural or under-served areas.
Introduction to Texas Medicaid
Texas Medicaid is a state and federally funded program that provides health benefits to eligible low-income individuals and families, including children, pregnant women, people with disabilities, and seniors. Designed to ensure access to essential health services, Texas Medicaid offers comprehensive coverage, including medical, dental, and mental health care, often referred to as behavioral health care.
In terms of mental health services, Texas Medicaid covers a wide range of treatments to support individuals with mental health needs. These services include evidence-based therapies such as cognitive behavioral therapy (CBT), family therapy, group therapy, and medication management. The program aims to promote recovery and resiliency, offering services tailored to meet the unique needs of each participant.
Who is eligible for Texas Medicaid?
Texas Medicaid provides health coverage to low-income individuals who meet specific eligibility criteria. To qualify, applicants must be Texas residents, U.S. citizens or eligible non-citizens, and fall within certain income thresholds based on their household size. Additionally, eligibility often depends on specific circumstances, such as pregnancy, disability, or the presence of dependent children in the household.
Special coverage for specific groups
Texas Medicaid includes special programs for certain populations:
- Children: Through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, children under 21 receive comprehensive preventive, diagnostic, and treatment services to address physical and mental health needs.
- Pregnant women: Pregnant individuals may qualify for Medicaid coverage that extends to prenatal, delivery, and postpartum care.
- People with disabilities: Specialized Medicaid programs provide tailored care for adults and children with disabilities, including therapies and support services.
Determining medical necessity
For therapy and other healthcare services to be covered, they must be deemed “medically necessary.” This means that the services must be necessary to prevent, diagnose, or treat a condition or its symptoms and align with accepted medical practices. A licensed healthcare provider assesses and documents medical necessity based on the individual’s health needs, ensuring that the treatment is appropriate and effective.
Does Texas Medicaid cover therapy?
Yes, Texas Medicaid typically covers therapy—including in-person and online therapy—as well as a wide range of mental health services that are designed to help with substance abuse, depression, anxiety, stress, relationship issues, OCD and more.
What therapy does Texas Medicaid cover?
Texas Medicaid insurance covers many types of therapy that serves as quality care options for many types of conditions. You need to confirm what types of therapy your specific Texas Medicaid plan covers, but in general the types of therapy Texas Medicaid typically covers includes:
- Individual therapy
- Family therapy
- Group therapy
- Skills training and rehabilitation
- Peer support services
- Crisis intervention services
- Psychosocial rehabilitation
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
Other types of therapy that Texas Medicaid may cover, depending on diagnosis, previous therapies, and your Texas Medicaid plan details:
- Applied behavior analysis (ABA)
- Substance use counseling
- Play therapy
- Electroconvulsive therapy (ECT)
Mental health services under Texas Medicaid are provided by licensed professionals such as psychiatrists, therapists, and counselors. Always verify that your chosen provider is in-network to ensure coverage.
Learn more about other types of therapy you might find when seeking mental health care, and be sure to double check your specific Texas Medicaid health plan, or reach out to Texas Medicaid directly, to understand what therapy may be covered by your Texas Medicaid insurance.
Medication coverage with Texas Medicaid
Texas Medicaid provides coverage for a wide range of psychiatric medications used to treat mental health conditions such as depression, anxiety, bipolar disorder, schizophrenia, and attention-deficit/hyperactivity disorder (ADHD). The types of psychiatric medications typically covered include:
- Antidepressants: For conditions like depression and anxiety disorders.
- Antipsychotics: Used to manage symptoms of schizophrenia, bipolar disorder, and other psychotic disorders.
- Mood stabilizers: Commonly prescribed for bipolar disorder to regulate mood swings.
- Anxiolytics: Medications to reduce symptoms of anxiety.
- Stimulants and non-stimulants: For the treatment of ADHD.
- Sedatives and sleep aids: When prescribed to manage sleep disturbances related to mental health conditions.
Prior authorization for high-cost or specialized medications
For certain high-cost or specialized psychiatric medications, prior authorization may be required. This process ensures the medication is medically necessary and that less expensive alternatives have been considered. Your healthcare provider will typically submit the required documentation to Texas Medicaid for review and approval.
Beneficiaries are encouraged to consult with their prescribing provider and Medicaid plan to confirm coverage details, including any copayments, refill limits, or requirements for generic alternatives.
What types of therapy does Texas Medicaid not cover?
Texas Medicaid covers many types of therapy which may help an individual with their mental health needs. However, there are some types of mental health services which are not covered by Texas Medicaid. These services include, but may not be limited to:
- Life coaching
- Therapies provided by unlicensed practitioners
- Alternative or experimental therapies
- Long-term psychoanalysis
- Couples counseling
- Educational testing or evaluations
- Therapeutic retreats or camps
- Cosmetic or lifestyle-related therapies
Does Texas Medicaid cover online therapy?
Yes, Texas Medicaid covers online therapy, also known as telehealth or virtual therapy, in addition to in-person therapy. This allows individuals to access mental health services from the comfort of their home, making care more convenient and accessible, particularly for those in rural or under-served areas.
Online therapy under Texas Medicaid makes mental health services more accessible to those facing barriers such as transportation challenges or geographical limitations. Always confirm specific coverage and requirements with your Medicaid plan before scheduling telehealth sessions.
Does Texas Medicaid cover out-of-network therapy?
Texas Medicaid primarily works with a network of approved, enrolled providers to deliver covered services. In most cases, therapy provided by an out-of-network therapist is not covered under Texas Medicaid. Beneficiaries are encouraged to seek care within the Medicaid provider network to ensure their therapy is eligible for coverage.
Key considerations for out-of-network therapy:
Exceptions: In rare cases, out-of-network therapy may be covered if (1) a required service is not available within the Medicaid network or (2) the provider has received prior authorization or a special arrangement from Texas Medicaid.
Prior Authorization: For out-of-network services to be considered, prior authorization from Medicaid is almost always required. This process includes documenting why in-network providers cannot meet the patient’s needs.
Additional Costs: If you choose an out-of-network therapist without prior approval, you may be responsible for the full cost of services.
To ensure your therapy is covered, always verify that your provider is in-network and confirm any exceptions directly with your Medicaid plan. If you are struggling to find a suitable in-network therapist, contacting your Medicaid plan representative for assistance is recommended.
How to check if your Texas Medicaid plan covers therapy
There are three main ways to find out if your Texas Medicaid plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your Texas Medicaid “summary of benefits”
On the summary of benefits (SOB), look for a row that references mental health, behavioral health, or substance abuse services, as well as “outpatient services” (because therapy is considered to be outpatient care).
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your Texas Medicaid plan does cover mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered”, then your Texas Medicaid plan does not cover mental health services such as therapy.
To learn more about how summary of benefits are structured, you can refer to this sample SOB from the Centers of Medicare & Medicaid Services website.
2. Contact Texas Medicaid directly
Contacting Texas Medicaid directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for Texas Medicaid, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the Texas Medicaid website to log into your account, and either chat or email a Texas Medicaid representative directly
3. Use a therapy provider like Grow Therapy
With Grow Therapy, you can search for mental health providers who are in-network with Texas Medicaid who are licensed in your state and provide both online therapy or in-person therapy. On Grow Therapy, you can browse our growing network of vetted therapists and use filters to search by age, specialty, gender, and more. Simply pick the therapist who meets your unique needs and book your first session.
When booking, you’ll be asked to enter your insurance information to verify eligibility and receive a cost estimate.
How much does Texas Medicaid therapy cost?
Most people insured by Texas Medicaid will either be fully covered by their plan or have to pay a small copay amount for therapy services. For the majority of clients, the cost of therapy under Texas Medicaid is minimal, with many qualifying for services at no cost.
Typical costs for therapy with Texas Medicaid:
Full coverage: Many beneficiaries, particularly children and individuals with disabilities, receive therapy services completely free of charge.
Copayments: In some cases, Texas Medicaid may require a small copay for therapy services. These copays are typically nominal, ranging from $0 to $5 per session, depending on the plan and the recipient’s eligibility category.
Medicaid is designed to reduce financial barriers to mental health care, ensuring that low-income individuals and families can access necessary treatment. Always check with your Medicaid plan or provider to confirm any potential costs for therapy services
Texas Medicaid therapy copay
When paying for therapy, your copay (or copayment) is an important cost you should know about.
The copay is a fixed amount you have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double check your copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to Texas Medicaid support directly.
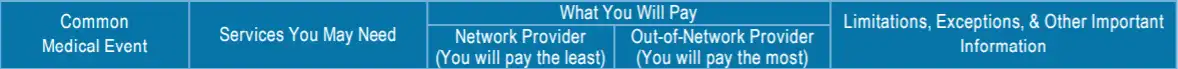
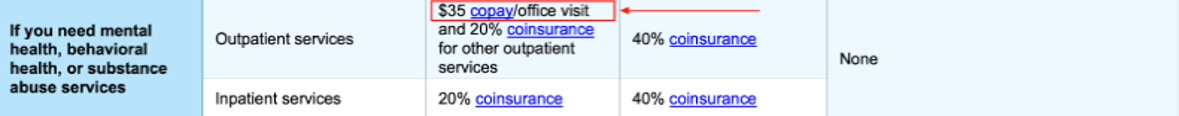
Sample image
Does Texas Medicaid require a referral to see a therapist?
Depending on your specific plan, Texas Medicaid may not require a referral to see a therapist or access mental health benefits. Many beneficiaries, especially those enrolled in Medicaid managed care plans such as STAR, STAR Kids, or STAR+PLUS, can often schedule therapy services directly with a Medicaid-approved provider. Verifying your plan’s rules will help ensure seamless access to therapy services covered under Texas Medicaid.
How to find a therapist covered by Texas Medicaid
Finding a therapist who accepts Texas Medicaid insurance is simpler than you might think. Whether you’re seeking counseling services for mental illness, need guidance as a caregiver, or are exploring services for children under the Children’s Health Insurance Program (CHIP), Texas Medicaid offers various resources to help you.
1. Contact Texas Medicaid customer service
One of the easiest ways to find a mental health professional covered by Texas Medicaid is by contacting their customer service. Representatives can guide Texans to local mental health authorities, case management programs, or health centers that offer Medicaid-covered inpatient or outpatient therapy.
To reach customer service:
- Call the hotline number on your Texas Medicaid ID card: This toll-free number connects you directly to Medicaid’s support team.
- Visit the Texas Medicaid website: Log into your account to access resources, live chat in English or Spanish, or send a message to a representative.
Customer service can provide a list of approved providers based on your location, specific needs, and coverage details, making it easier to find the right therapist for you.
2. Other resources
Texas Health and Human Services (HHS) also works with local mental health authorities to provide community services, counseling services, and waiver programs for individuals with unique needs. These programs support a wide range of populations, including children, adults, and seniors, ensuring access to essential care throughout the state.
3. Use Grow Therapy
You can search for an Texas Medicaid therapist using Grow Therapy. Just select your state, your Texas Medicaid pan, and any specializations you’re looking for. You’ll then see a list of providers you can choose from and reach out to schedule a session.
What do terms like deductible, copay, and coinsurance mean?
Navigating the insurance system—especially when you’re in need of mental health support—can be challenging and confusing. For help, please visit our Understanding health insurance article.
Navigating common issues with Texas Medicaid health coverage
While Texas Medicaid offers extensive mental health coverage, beneficiaries may face challenges such as denied claims or pre-authorization requirements. Here’s how to troubleshoot these and other common issues.
Denied claims
Denied claims often arise when Medicaid determines a service is not covered, lacks required documentation, or was provided by an out-of-network provider.
What to try: First, review the denial letter or explanation of benefits (EOB) carefully to understand the reason. Contact your Medicaid plan for clarification and, if you believe the service should be covered, file an appeal. Include supporting documentation, such as treatment plans or a letter of medical necessity from your provider. If needed, consider reaching out to a Medicaid ombudsman or patient advocate for guidance through the appeals process.
Needing pre-authorization
Some therapy services or medications require pre-authorization to ensure they are medically necessary.
What to try: Confirm with your Medicaid plan or therapist if pre-authorization is required before starting treatment. If it is, work with your provider to submit the necessary documentation, including evidence that justifies the need for the service. Follow up with your plan to check the status of the request and provide additional information promptly if asked.
Provider availability
Finding an in-network therapist can sometimes be challenging.
What to try: Use the Medicaid provider directory to search for therapists in your area, or contact your Medicaid plan’s member services for help locating a provider with availability. Be flexible with appointment times or consider telehealth options if in-person services are limited.
Coverage confusion
Understanding what your plan covers can be complicated.
What to try: Review your plan benefits through the Your Texas Benefits portal or speak with your Medicaid plan’s customer service team to clarify coverage details and avoid unexpected issues.
By addressing these challenges proactively and using the available resources, beneficiaries can make the most of their Texas Medicaid mental health benefits.
Making the most of your mental health coverage with Texas Medicaid
To maximize your mental health benefits under Texas Medicaid, stay informed about your plan’s coverage, including available services and any policy changes. Regularly reviewing plan details ensures you’re prepared to access care without surprises.
Be proactive in addressing mental health concerns by seeking help early and advocating for yourself when challenges arise, such as denied claims or provider shortages. Use resources like Medicaid ombudsmen or member services for support.
Finally, explore alternative treatments and preventive care options, such as skills training or peer support, to enhance your overall wellness and recovery journey. By staying engaged, you can make the most of your Medicaid benefits.

