The costs of mental health care, especially therapy, can add up quickly. Fortunately, Indiana Medicaid covers a range of mental health services that can help reduce out-of-pocket costs for eligible members. This article breaks down what’s included in Indiana Medicaid’s mental health coverage, from counseling to addiction treatment, and explains how to navigate any limitations. Understanding your plan’s benefits and knowing how to access services through approved providers can make a difference in your care. Explore how to make the most of Indiana Medicaid for affordable, accessible mental health support.
Key takeaways
- Indiana Medicaid provides coverage for mental health services, including therapy, substance use treatment, counseling, and more.
- Commonly covered therapies include individual counseling, cognitive behavioral therapy (CBT), trauma-focused therapy, and addiction counseling.
- Specific therapies may require prior authorization or medical necessity verification.
- Copays typically ranging from $0 to $20 per session. Costs vary by plan, and members should verify coverage details before seeking treatment.
- To access services, members should use Indiana Medicaid’s provider directory or contact Medicaid customer service to find in-network therapists.
Introduction to Indiana Medicaid
Indiana Medicaid is a program that’s funded jointly by the state and federal government to provide health benefits for low-income individuals, families, seniors, and people with disabilities in Indiana. Coverage includes medical, dental, and mental health (behavioral health) care to support various health needs.
For mental health, Indiana Medicaid covers services like individual counseling, substance use disorder treatment, peer support services, and more. This helps members access essential treatment options for managing mental and behavioral health conditions.
Indiana Medicaid works closely with the Division of Mental Health and Addiction (DMHA) to deliver behavioral health services that align with state standards and support improved mental health outcomes for residents.
Who is eligible for Indiana Medicaid?
Eligibility for Indiana Medicaid depends on income level, Indiana residency, and specific health needs. Generally, adults with low incomes, families, seniors, pregnant women, and individuals with disabilities may qualify.
Indiana Medicaid also offers special coverage for groups with unique health needs, including children who receive comprehensive care through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, and pregnant women who have access to full medical and prenatal support.
Does Indiana Medicaid cover therapy?
Yes, thanks to the Affordable Care Act, which expanded the scope of Medicaid’s coverage nationwide, Indiana Medicaid typically covers therapy. Coverage includes in-person and online therapy, as well as a wide range of mental health services that are designed to help with substance abuse, depression, anxiety, stress, relationship issues, OCD, and more.
What therapy does Indiana Medicaid cover?
Indiana Medicaid insurance covers many types of therapy that serve as quality care options for many conditions. You need to confirm what types of therapy your specific Indiana Medicaid plan covers, but in general the types of therapy Indiana Medicaid typically covers includes:
- Addiction counseling and substance use disorder treatment
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Trauma-focused therapy
- Individual counseling
- Family therapy
- Group therapy
Other types of therapy that Indiana Medicaid may cover, depending on diagnosis, previous therapies, and your Indiana Medicaid plan details:
- Ketamine and esketamine (Spravato)
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation (TMS)
- Biofeedback therapy (coverage may vary)
Indiana Medicaid covers mental health services from the following types of providers:
- Licensed marriage and family therapists (LMFT)
- Licensed Clinical Addiction Counselors (LCAC)
- Licensed Mental Health Counselors (LMHC)
- Licensed Clinical Social Workers (LCSW)
- Certified Peer Support Specialists
- Psychologists
- Psychiatrists
- Advanced Practice Registered Nurses (APRN) with psychiatric certification
- Primary Care Physicians (PCP) (for general mental health assessments and medication management)
Learn more about other types of therapy you might find when seeking mental health care, and be sure to double check your specific Indiana Medicaid health plan, or reach out to Indiana Medicaid directly, to understand what therapy may be covered by your Indiana Medicaid insurance.
Determining medical necessity
For Indiana Medicaid to cover therapy, services must be deemed “medically necessary.” This means that a provider, such as a therapist or counselor, assesses the need based on a health condition that requires treatment, ensuring the service is appropriate and likely to benefit the patient’s health or quality of life.
Medication coverage with Indiana Medicaid
Indiana Medicaid covers a range of psychiatric medications to support mental health treatment, including commonly prescribed antidepressants, antipsychotics, mood stabilizers, anti-anxiety medications, and ADHD medications. Coverage typically includes generic and brand-name options, though the specific formulary may vary by Medicaid plan.
For high-cost or specialized medications, such as newer antipsychotics or medications like esketamine (Spravato), prior authorization is usually required. This means your provider must demonstrate medical necessity for the medication, and approval from Medicaid may be needed before coverage applies.
What types of therapy does Indiana Medicaid not cover?
Indiana Medicaid covers many types of therapy which may help an individual with their mental health needs. However, there are some types of mental health services which are not covered by Indiana Medicaid. These services include, but may not be limited to:
- Hypnotherapy: Hypnotherapy uses hypnosis to help people with their mental health problems. Although some people find it helpful, Indiana Medicaiddoes not believe it is a reliable or effective treatment for mental health issues.
- Non-traditional therapy: Non-traditional therapy, such as biofeedback therapy, aims to help people control their body’s response to stress and anxiety by giving them feedback about their body’s functions, like their heart rate or blood pressure. Indiana Medicaiddoes not cover this type of therapy because they do not think there is enough evidence to prove that it’s an effective form of treatment.
- Life coaching: Services such as life coaching or motivational counseling are not covered, as they do not meet Medicaid’s criteria for medical or therapeutic necessity.
- Art and music therapy: While these can be valuable in a mental health context, Indiana Medicaid does not cover art or music therapy unless it is part of an approved therapeutic program that meets strict clinical guidelines.
Does Indiana Medicaid cover online therapy?
Yes, Indiana Medicaid covers online therapy, also known as telehealth or virtual therapy, in addition to in-person therapy sessions. Virtual therapy is available for various services, including individual counseling, family therapy, psychiatric evaluation, and medication management.
- Approved providers: Online therapy must be provided by a licensed Medicaid-approved provider. Not all providers may offer telehealth options, so checking with your chosen provider is essential.
- Eligible services: While many standard therapy services are covered via telehealth, more intensive treatments like group therapy or specialized therapies (e.g., addiction treatment or behavioral therapies requiring in-person interaction) may be limited in availability through virtual means.
Search for therapists who accept Indiana Medicaid
Does Indiana Medicaid cover out-of-network therapy?
Indiana Medicaid does not cover out-of-network therapists. If you want to see an out-of-network mental healthcare provider with Indiana Medicaid, it will likely cost more than seeing an in-network provider. You will have to pay out-of-pocket and should check beforehand with your individual plan to see if you’re able to file for any kind of reimbursement from Indiana Medicaid. If you have questions about out-of-network therapy coverage, please refer to your Indiana Medicaid summary of benefits (SOB) as described below, or contact Indiana Medicaid directly.
How to check if your Indiana Medicaid plan covers therapy
There are two main ways to find out if your Indiana Medicaid plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your Indiana Medicaid “summary of benefits”
On the summary of benefits (SOB), look for a row that references mental health, behavioral health, or substance abuse services, as well as “outpatient services” (because therapy is considered to be outpatient care).
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your Indiana Medicaid plan does cover mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered,” then your Indiana Medicaid plan does not cover mental health services such as therapy.
To learn more about how Summary of Benefits are structured, you can refer to this sample SOB from the Centers of Medicare & Medicaid Services website.
2. Contact Indiana Medicaid directly
Contacting Indiana Medicaid directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for Indiana Medicaid, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the Indiana Medicaid website to log into your account, and either chat or email an Indiana Medicaid representative directly
How much does Indiana Medicaid therapy cost?
Most people who are insured by Indiana Medicaid will either be fully covered by their plan, or have to pay a small copay amount. For most clients, the average cost of Indiana Medicaid for therapy is $0 – $20 per session, after the deductible has been met. For those who haven’t met their deductible yet, the typical range of therapy sessions is $50 – $200 per session.
These are average ranges, however, so if you are insured by Indiana Medicaid the cost of therapy will depend on your plan’s specific coverage — you should always confirm your out-of-pocket costs before your appointment.
Indiana Medicaid therapy copay
When paying for therapy, your copay (or copayment) is an important cost you should know about.
The copay is a fixed amount you have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double check your copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to Indiana Medicaid support directly.
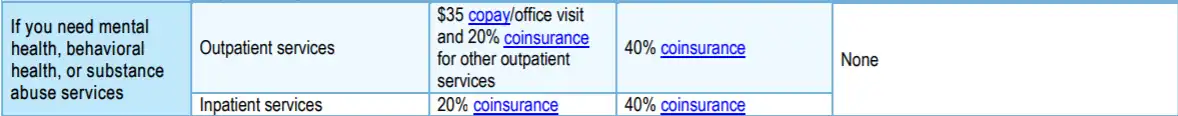
Example Only
What do terms like deductible, copay, and coinsurance mean?
Navigating the insurance system — especially when you’re in need of mental health support — can be challenging and confusing. For help, please visit our Understanding health insurance article.
Does Indiana Medicaid require a referral to see a therapist?
Depending on your specific plan, Indiana Medicaid may or may not require a referral to access therapy and mental health benefits. Generally, managed care plans like Hoosier Care Connect or the Healthy Indiana Plan (HIP) often require members to go through their Primary Medical Provider (PMP) for a referral, especially for specialized mental health services. However, some services may be accessed directly without a referral.
For the most accurate information, refer to your Indiana Medicaid policy or visit the Indiana Medicaid website for details.
How to find a therapist covered by Indiana Medicaid
Finding a therapist who accepts Indiana Medicaid insurance is easier than you might think.
1. Indiana Medicaid directory of therapists
Indiana Medicaid offers an online provider directory where you can search for mental health professionals who accept Medicaid insurance. This directory allows you to filter by location, specialization, provider availability, and more—and some listings may include provider reviews. You can search for community mental health centers as well. Using this tool can streamline your search, helping you find in-network therapists in your area without needing to call multiple offices.
2. Contact Indiana Medicaid customer service
If you prefer personal assistance, Indiana Medicaid customer service can help you find a mental health provider who accepts Medicaid. Call the customer service number on your Medicaid card(or that of a loved one), and a representative can guide you to in-network providers near you, answer questions about specific therapists, or help with any additional coverage questions.
3. Use a therapy provider like Grow Therapy
With Grow Therapy, you can search for mental health providers who are in-network with Indiana Medicaid who are licensed in your state and provide both online therapy or in-person therapy. On Grow Therapy, you can browse our growing network of vetted therapists and use filters to search by age, specialty, gender, and more. Simply pick the therapist who meets your unique needs and book your first session. At this time, providers with Grow Therapy are accepting Humana Dual Medicare & Medicaid, Managed Health Services Managed Medicaid, and UnitedHealthcare/Optum Medicaid in Indiana.
Search for therapists who accepts Indiana Medicaid
When booking, you’ll be asked to enter your insurance information to verify eligibility and receive a cost estimate.
Navigating common issues with Indiana Medicaidhealth coverage
Here’s a step-by-step guide to troubleshoot common issues around mental health coverage with Indiana Medicaid, including what to do if you face denied claims, pre-authorization requirements, or other obstacles.
Denied claims
A claim denial may occur if a therapy or mental health service doesn’t meet Indiana Medicaid’s coverage criteria or is billed incorrectly by the provider.
What to try
First, contact your provider’s billing office to verify that the service was billed correctly. Next, reach out to Indiana Medicaid customer service to review the reason for the denial. If you believe the denial is incorrect, you can file an appeal by following the instructions on your Medicaid Summary of Benefits or on the Indiana Medicaid website. Appeals generally require documentation from your provider supporting the medical necessity of the service.
Needing pre-authorization
Some mental health services, especially specialized therapies or high-cost treatments, require prior authorization from Indiana Medicaid to confirm they meet medical necessity standards.
What to try
Ask your therapist or mental health provider to submit a prior authorization request on your behalf. Ensure that they provide all required documentation to justify the treatment’s necessity. If authorization is delayed or denied, contact Indiana Medicaid to understand the reason and ask about resubmission options or alternative therapies that may not need prior authorization.
Out-of-network services
Indiana Medicaid generally requires using in-network providers, so seeking care outside the network may lead to denied claims or higher out-of-pocket costs.
What to try
Before seeking out-of-network care, check your provider directory for in-network options. If in-network providers are unavailable or don’t meet your needs, contact Medicaid customer service to explore options for network exceptions or reimbursement requests.
Service limitations or frequency caps
Certain therapies or services may have limits on the number of sessions allowed annually or may not be covered for extended periods.
What to try
Speak with your provider about adjusting your treatment plan to fit within Medicaid’s coverage limits. If additional sessions are essential, ask your provider to document medical necessity and submit a request for extended coverage to Medicaid.
Navigating these issues often involves collaboration with both your provider and Indiana Medicaid, ensuring that you get the necessary coverage and support for your mental health needs.
Making the most of your mental health coverage with Indiana Medicaid
Understanding and making full use of your mental health benefits under Indiana Medicaid can be key to maintaining well-being and accessing essential support. Regularly reviewing your plan details and staying informed about any changes to coverage helps ensure that you’re prepared to take advantage of the resources available.
Being proactive with your mental health care, including seeking help early and advocating for yourself if you encounter obstacles, is essential for long-term wellness. Don’t hesitate to reach out for assistance with Medicaid navigation, and remember to explore alternative treatments or preventive options, such as counseling, wellness programs, and stress management resources. Taking an active role in your mental health journey can help you fully leverage your Medicaid benefits for comprehensive care.

