CBT-i, which stands for cognitive behavioral therapy for insomnia, is a form of psychotherapy designed to help people overcome sleep disorders. It works by identifying and addressing the thought patterns, behaviors, and habits that interfere with falling and staying asleep. The goal of CBT-i is to improve sleep quality and duration by teaching techniques to manage sleep-related stress and anxiety. This helps people develop healthy sleep habits and regain control over their sleep, without relying on medication.
What are the origins of cognitive behavioral therapy for insomnia (CBT-i)?
Developed in the 1970’s by Dr. Arthur Spielman and other sleep researchers, CBT-i was created as a non-medication treatment for chronic insomnia. It focuses on breaking the cycle of poor sleep through practical strategies and better management of unhelpful thoughts that disrupt rest. Since its development, CBT-i has become one of the most well-researched and effective treatments for insomnia, with studies showing it helps people of all ages fall asleep faster, stay asleep longer, and improve their overall quality of life.
When is cognitive behavioral therapy for insomnia (CBT-i) used?
Cognitive behavioral therapy for insomnia (CBT-i) is primarily used to treat individuals with insomnia, but can be adapted for group therapy. In a group setting, participants come together to share experiences, offer support, and apply the same sleep-improving interventions. Whether individually or in a group, CBT-i helps people understand the underlying factors affecting their sleep and teaches practical techniques to address them.
While CBT-i is not a treatment for mental health disorders like anxiety or depression, it has been shown to improve symptoms of these conditions since sleep plays a significant role in overall mental well-being. By improving sleep quality, CBT-i can help alleviate symptoms of a range of mental health concerns, such as:
- Intrusive thoughts, which are often experienced by individuals with anxiety that interfere with sleep.
- Mood stabilization and support for individuals with depression through better sleep.
- Pain management, as improved sleep quality can contribute to more effective management of chronic pain.
- PTSD, which can lead to cycles of sleep disturbances which then worsen trauma-related symptoms
Though CBT-i is often used alongside other treatments for mental health conditions, its primary benefit is improving sleep. This, in turn, has significant, far-reaching effects on overall well-being.
How does cognitive behavioral therapy for insomnia (CBT-i) work?
CBT-i helps retrain your brain and teaches new behaviors to make sleep easier. For example, many people with insomnia experience anxiety or panic about not sleeping, which only worsens the problem. CBT-i challenges these worries and fosters a more relaxed mindset toward sleep.
The therapy also focuses on changing habits that interfere with sleep. For instance, if you stay in bed when you’re not sleeping or check your phone before bed, CBT-i teaches you to break those habits. CBT-i encourages people to set a consistent bedtime, reduce caffeine intake, or engage in calming activities like reading or stretching before bed. Over time, these small changes help your brain and body associate the bed with sleep, not anxiety.
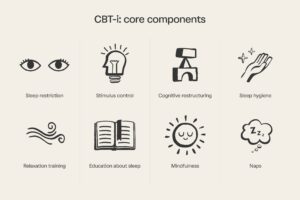
There are eight core components of CBT-i that work together to improve sleep quality:
- Sleep restriction – Although it can seem counterintuitive, the time spent in bed is initially reduced to match the actual sleep time, which helps improve sleep efficiency. For example, if you’re lying in bed for 8 hours but only sleeping for 4, you might start by reducing the time spent in bed to 5 hours. As sleep quality improves, the time spent in bed is gradually increased.
- Stimulus control – Breaks the association between your bed and wakefulness. If you can’t sleep, you leave the bed and return when you feel sleepy, helping your brain link your bed with sleep.
- Cognitive restructuring – Identifies and challenges negative thoughts about sleep that cause anxiety, replacing them with more positive, sleep-promoting thoughts.
- Sleep hygiene – Establishes lifestyle changes that promote better sleep, such as a consistent sleep schedule, reducing caffeine, and creating a restful environment (dark, cool, quiet).
- Relaxation training – Uses techniques like progressive muscle relaxation or deep breathing to reduce tension and anxiety, making it easier to fall asleep.
- Education about sleep – Teaches about the sleep cycle and factors that influence it, reducing anxiety and helping individuals approach sleep more calmly.
- Mindfulness – Some CBT-i approaches include mindfulness practices to help manage intrusive thoughts that interfere with sleep and improve relaxation.
- Naps – Manage naps by either avoiding them or ensuring they don’t disrupt nighttime sleep. If naps are taken, they should be earlier in the day.
These components of CBT-i help you develop healthier sleep habits, reduce anxiety about sleep, and improve overall sleep quality.
What is cognitive behavioral therapy for insomnia (CBT-i) like?
In the first session, your therapist will ask about your sleep patterns, the onset of your sleep problems, what you’ve already tried to improve your sleep, and what has or hasn’t worked. They’ll also inquire about your daytime and evening routines, diet, beverage intake (e.g., caffeine, alcohol), and sleep environment (e.g., room conditions). This information helps the therapist assess your sleep quality, identify challenges, and create a personalized treatment plan.
Just like in cognitive behavioral therapy (CBT) for other mental health challenges, CBT-i involves exploring how your thoughts (cognitions), feelings, and behaviors interact — but with a focus on how they affect your sleep. Beyond the cognitive element, CBT-i also helps you make practical changes to your life that improve sleep quality, such as adjusting your sleep schedule, addressing habits that interfere with sleep, or incorporating relaxation techniques (e.g., progressive muscle relaxation).
CBT-i often involves completing tasks — or “homework” — between sessions. You might track your sleep patterns in a sleep diary, engage in sleep restriction, monitor caffeine and alcohol intake, or practice sleep hygiene techniques (e.g., creating a wind-down routine). CBT-i is most effective when these strategies are practiced between sessions, allowing time for reflection and adjustments. In the end, CBT-i combines understanding your sleep challenges with practical strategies to improve both the quality and duration of your sleep.
How long does CBT-i take?
Compared to other psychotherapies CBT-i is a short-term treatment, usually involving 5 to 8 sessions, each lasting 50 minutes, held weekly or biweekly.
Is CBT-i effective?
CBT-i is an effective treatment for insomnia, with strong research supporting its success. Studies consistently show that CBT-i improves both the quality and quantity of sleep. For instance, a large systemic review that analyzed outcomes of 37 treatment studies and included over 2,000 participants found that CBT-i reliably improves sleep for individuals with insomnia. Additionally, a review and meta analysis of randomized controlled trials, found that the benefits of CBT-i lasted for months after treatment, with participants continuing to experience better sleep in the long-term.
Unlike sleeping pills, which can lose effectiveness and cause side effects, CBT-i addresses the root causes of sleep problems, leading to more lasting improvements. This evidence-based approach has made CBT-i the first-line treatment recommended by sleep medicine specialists and healthcare providers, as outlined in the American Academy of Sleep Medicine guidelines.
How to find a clinician who practices cognitive behavioral therapy for insomnia (CBT-i)
If you think cognitive behavioral therapy for insomnia might be right for you, it’s important to speak with a licensed and experienced clinician. There are many types of mental health care providers who practice CBT-i, including licensed marriage and family therapists (LMFTs), licensed clinical social workers (LCSWs), psychologists, psychiatrists, psychiatric nurses, licensed professional counselors (LPCs), licensed mental health counselors (LMHCs) and more.
On top of finding someone specializing in CBT-i, you want to make sure they meet your other needs. For example, if symptoms of trauma are contributing to your sleep problems, you may want to find a CBT-i therapist who also specializes in post-traumatic stress disorder (PTSD). In addition, finding a therapist who accepts your insurance can make therapy much more affordable.
You can find a therapist who accepts your insurance and specializes in CBT-i by using Grow Therapy. After filtering for your location, insurance, and needs, you can then select “Cognitive Behavioral Therapy for Insomnia (CBT-i)” from the “Treatment methods” drop-down.