Mental health care can be expensive, and the cost of therapy sessions can add up fast. Luckily, if you’re covered by Georgia Medicaid, your mental health care may be covered. This article helps you understand what’s covered, what’s not, and how to use your Georgia Medicaid coverage for mental health care.
Key takeaways
- Georgia Medicaid provides mental health services including outpatient therapy, medication management, inpatient care, and crisis intervention.
- Services are available for various conditions, such as anxiety, depression, trauma, and substance use disorders.
- Georgia Medicaid covers a range of therapies, including cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and family and group therapy.
- For most beneficiaries, the cost of therapy ranges from $0–75 per session, depending on the plan’s specific coverage.
Introduction to Georgia Medicaid
Georgia Medicaid is a joint state and federal program that provides health coverage to low-income individuals and families in Georgia. The program serves a range of populations, including children, pregnant women, elderly individuals, people with disabilities, and low-income adults who meet certain eligibility requirements. Georgia Medicaid is operated by the Georgia Department of Community Health (DCH).
Georgia Medicaid covers a wide range of medical services, including preventive care, hospital stays, doctor visits, and prescriptions. In addition to general medical services, Georgia Medicaid also provides coverage for dental care and mental health services, often referred to as behavioral health services.
Georgia Medicaid offers comprehensive mental health care coverage to individuals who need support for behavioral or emotional challenges. These services include all levels of care, including outpatient therapy, medication management, intensive outpatient programs, rehabilitation services, and inpatient psychiatric hospitalization
Who is eligible for Georgia Medicaid?
Eligibility for Georgia Medicaid is based on several factors, including income thresholds, state residency, and specific health needs. To qualify, individuals must live in Georgia and meet certain financial criteria, which vary depending on family size and income level. Specific groups such as pregnant women, children, seniors, and individuals with disabilities may qualify under different income limits and eligibility categories. Additionally, Georgia Pathways to Coverage™ offers a new Medicaid coverage option for adults ages 19-64 with incomes up to 100% of the federal poverty level (FPL), as long as they meet certain activity requirements such as working or receiving job training.
Income thresholds play an important role in whether or not someone is eligible for Medicaid in Georgia. The program uses the FPL to set these limits, and the thresholds vary depending on group someone is in. For example, pregnant women and children generally have higher income limits, making it easier for them to qualify.
Certain populations get special coverage through Georgia Medicaid.
- Children are entitled to services through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program, which ensures access to preventive health services and necessary treatments. The program also offers help to kids in foster care.
- Pregnant women benefit from prenatal and childbirth-related care
- Individuals with disabilities may qualify for additional supports, such as long-term care or home- and community-based services.
- Caregivers and community providers of care receive additional support support
- Young people in psychiatric residential treatment facilities (PRTFs) receive comprehensive mental health care when necessary under Medicaid’s “Psych under 21” benefit
Does Georgia Medicaid cover therapy?
Yes, Georgia Medicaid typically covers therapy — including in-person and online therapy — as well as a wide range of mental health services that are designed to help with substance abuse, depression, anxiety, stress, relationship issues, trauma, and more.
The Affordable Care Act, which enabled Medicaid expansion, requires Medicaid plans to include mental health and substance use disorder services as essential health benefits. The Affordable Care Act means that beneficiaries have access to a comprehensive array of treatments, from counseling and psychotherapy to medication management and inpatient services.
For Medicaid to cover mental health or other medical services, they must be considered “medically necessary.” This means that therapy or treatment is needed to prevent, diagnose, or treat a condition or its symptoms. Healthcare providers determine medical necessity based on the individual’s condition, and services must align with accepted medical standards to be covered by Medicaid.
Under Medicaid’s coverage, eligible individuals can access these services through licensed mental health professionals without significant out-of-pocket costs, making mental health care more accessible for those in need.
What therapy does Georgia Medicaid cover?
Georgia Medicaid insurance covers many types of therapy to treat a variety of conditions. Coverage can vary from plan to plan, but in general, the types of therapy Georgia Medicaid covers include:
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Therapy for adolescents
- Family therapy
- Group therapy
- Therapy for ADHD
- Crisis intervention
- Medication management
Other types of therapy that Georgia Medicaid may cover, depending on diagnosis, previous therapies, and your Georgia Medicaid plan details:
- Ketamine and esketamine (Spravato)
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation (TMS)
Georgia Medicaid covers mental health services from providers with the following accreditation:
- Licensed Marriage and Family Therapists (LMFTs)
- Licensed Clinical Social Workers (LCSWs)
- Licensed Professional Counselors (LPCs)
- Certified Addiction Counselors (CACs)
- Psychologists
- Psychiatrists
- Nurse Practitioners
Be sure to double check your specific Georgia Medicaid health plan, or reach out to Georgia Medicaid directly, to understand what therapy may be covered by your Georgia Medicaid insurance.
Search for therapists who accept Georgia Medicaid
Medication coverage with Georgia Medicaid
Georgia Medicaid covers a wide range of psychiatric medications to help manage mental health conditions, including depression, anxiety, bipolar disorder, schizophrenia, opioid use disorder, and substance use. Commonly covered medications include antidepressants, antipsychotics, mood stabilizers, and anti-anxiety medications. Generic versions of psychiatric medications are often available at no additional cost, reducing the financial burden on beneficiaries while maintaining effective treatment.
Certain brand-name medications or newly developed psychiatric drugs may not be covered, limiting options for individuals who do not respond well to more standard treatments. Access to specific medications may depend on state formulary decisions, which may vary or change over time, impacting availability.
Prior authorization for high-cost or specialized medications
For high-cost or specialized psychiatric medications, Georgia Medicaid may require prior authorization. This process ensures that these medications are medically necessary and appropriate for the patient’s condition. Healthcare providers must submit a request with clinical justification, especially for expensive drugs or those outside of typical treatment guidelines.
What types of therapy does Georgia Medicaid not cover?
There are some types of mental health services which are not covered by Georgia Medicaid. These services include, but may not be limited to:
- Hypnotherapy: Hypnotherapy uses hypnosis to help people with their mental health problems. Although some people find it helpful, Georgia Medicaid does not believe it is a reliable or effective treatment for mental health issues.
- Non-traditional therapy: Non-traditional therapy, such as biofeedback therapy, aims to help people control their body’s response to stress and anxiety by giving them feedback about their body’s functions, like their heart rate or blood pressure. Georgia Medicaid does not cover this type of therapy because they do not think there is enough evidence to prove that it’s an effective form of treatment.
- Life coaching: Life coaching focuses on personal development and goal setting rather than addressing diagnosable mental health disorders. Since it is not considered a medical or clinical service, Georgia Medicaid does not cover life coaching.
- Psychoanalysis: While Georgia Medicaid covers most mainstream forms of psychotherapy, psychoanalysis, which involves long-term, intensive exploration of unconscious thoughts and feelings, is typically not covered due to its high cost and limited use in evidence-based treatments.
- Recreational therapy: This type of therapy involves activities such as art, music, or animal therapy to improve emotional well-being. While beneficial for some individuals, these therapies are often excluded from Georgia Medicaid coverage unless provided as part of a broader therapeutic program.
- Experimental therapies: Any therapies that are considered experimental or not yet widely accepted as evidence-based practices in the mental health field are typically not covered by Georgia Medicaid. This may include newer or unconventional treatment methods that lack sufficient clinical evidence.
Does Georgia Medicaid cover online therapy?
Yes, Georgia Medicaid covers both online therapy, also known as telehealth or virtual therapy. This allows beneficiaries to receive mental health care remotely, providing flexibility and convenience, especially for individuals with transportation barriers or those living in rural areas.
- Telehealth eligibility: Online therapy must be provided by a Medicaid-approved mental health professional, such as a licensed therapist, psychologist, or psychiatrist.
- Covered services: Telehealth services include individual therapy, group therapy, and medication management for mental health conditions. These services are generally covered at the same rate as in-person visits.
- Technology requirements: Beneficiaries need access to a device (such as a smartphone, tablet, or computer) and an internet connection to participate in online therapy.
- Exceptions: Some complex mental health conditions or assessments may still require in-person visits. Additionally, certain treatments, such as those involving physical interventions, may not be suitable for telehealth.
This coverage ensures that beneficiaries can access mental health support from the comfort of their own homes, enhancing the availability of care across the state.
Does Georgia Medicaid cover out-of-network therapy?
Georgia Medicaid does not typically cover out-of-network therapists. If you want to see an out-of-network mental healthcare provider with Georgia Medicaid, it will likely cost more than seeing an in-network provider. You may have to pay out of pocket, and you should check beforehand to see if you will be able to file for any kind of reimbursement from Georgia Medicaid. If you have questions about out-of-network therapy coverage, please refer to your Georgia Medicaid summary of benefits (SOB) as described below, or contact Georgia Medicaid directly.
How to check if your Georgia Medicaid plan covers therapy
There are two main ways to find out if your Georgia Medicaid plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your Georgia Medicaid “summary of benefits”
On the summary of benefits (SOB), look for a row that references mental health, behavioral health, or substance abuse services, as well as “outpatient services” (because therapy is considered to be outpatient care).
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your Georgia Medicaid plan does cover mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered,” then your Georgia Medicaid plan does not cover mental health services such as therapy.
To learn more about how Summary of Benefits are structured, you can refer to this sample SOB from the Centers of Medicare & Medicaid Services website.
2. Contact Georgia Medicaid directly
Contacting Georgia Medicaid directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for Georgia Medicaid, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the Georgia Medicaid website to log into your account, and either chat or email an Georgia Medicaid representative directly
How much does Georgia Medicaid therapy cost?
Most people who are insured by Georgia Medicaid will either be fully covered by their plan, or have to pay a small copay amount. For most clients, the average cost of Georgia Medicaid for therapy is $0-75 per session after the deductible has been met. For those who haven’t met their deductible yet, you may have to pay the therapist’s full session rate.
These are average ranges, however, so if you are insured by Georgia Medicaid the cost of therapy will depend on your plan’s specific coverage — you should always confirm your out-of-pocket costs before your appointment.
Georgia Medicaid therapy copay
When paying for therapy, your copay (or copayment) is an important cost you should know about.
The copay is a fixed amount you have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double check your copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to Georgia Medicaid support directly.
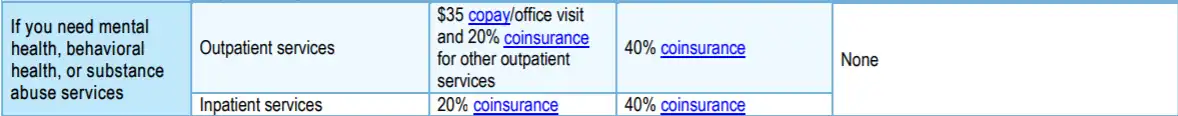
Example Only
What do terms like deductible, copay, and coinsurance mean?
Navigating the insurance system — especially when you’re in need of mental health support — can be challenging and confusing. For help, please visit our Understanding health insurance article.
Does Georgia Medicaid require a referral to see a therapist?
Depending on your specific plan, Georgia Medicaid generally does not require a referral to see a therapist or access mental health services. However, it’s important to verify details about your specific Medicaid plan to ensure whether a referral from a primary care physician (PCP) is needed before scheduling an appointment with a mental health provider. Requirements may vary depending on the service or provider. For the most accurate information, visit the official Georgia Medicaid website or contact their customer service.
How to find a therapist covered by Georgia Medicaid
Finding a therapist who accepts Georgia Medicaid insurance may be easier than you think. Several options can help you locate an in-network mental health provider, saving time and ensuring your therapy sessions are covered.
1. Georgia Medicaid Provider Directory
Georgia Medicaid offers an online provider portal where you can search for mental health professionals in your area. These directories typically allow you to filter providers by location, specialization (such as anxiety, depression, or family therapy), and availability.
2. Contact Georgia Medicaid Customer Service
You can also contact Georgia Medicaid’s customer service for help finding a mental health professional. Representatives are available by phone or through the Medicaid website to assist you in locating therapists within your network, based on your location and specific needs. They can also provide details about your mental health benefits, including whether a referral is required and what services are covered under your plan.
3. Use a therapy provider like Grow Therapy
With Grow Therapy, you can search for licensed mental health providers who are in-network with Georgia Medicaid and provide both in-person and online therapy. At this time, Grow Therapy works with providers who accept Humana Dual Medicaid, Peach State Health Plan Medicaid, and Peach State Health Plan Managed Medicaid.
On Grow Therapy, you can browse our growing network of vetted therapists and use filters to search by age, specialty, gender, and more. Simply pick the therapist who meets your unique needs and book your first session.
Search for therapists who accept Georgia Medicaid
When booking, you’ll be asked to enter your insurance information to verify eligibility and receive a cost estimate.
Navigating common issues with Georgia Medicaid health coverage
Dealing with issues related to Georgia Medicaid mental health coverage can be frustrating, but knowing how to troubleshoot common problems can help you maintain access to necessary care. Below is a guide to addressing common challenges:
Denied claims
Denied claims occur when Georgia Medicaid refuses to cover a service or treatment, often due to incomplete paperwork, incorrect coding, or because the service is deemed “not medically necessary.”
What to try
Start by reviewing the Explanation of Benefits (EOB) to determine the reason for the denial. If the denial is due to incomplete or incorrect information, work with your healthcare provider to correct and resubmit the claim. If the denial is because the service was deemed not medically necessary, consider filing an appeal. In the appeal, include additional documentation from your provider justifying the necessity of the treatment or service. Stay in contact with Medicaid throughout the process to ensure all steps are followed.
Needing pre-authorization
Certain mental health services, especially high-cost treatments or specialized therapies, may require pre-authorization. This means Medicaid must approve the service before it is provided.
What to try
Request that your mental health provider submit a pre-authorization request to Georgia Medicaid on your behalf. Ensure that your provider includes comprehensive documentation explaining why the treatment is medically necessary. Regularly check with both your provider and Georgia Medicaid to track the status of the request. If the request is denied, you may have the option to appeal the decision with further justification.
Network limitations
Some beneficiaries find that there are few mental health providers in their area who accept Georgia Medicaid.
What to try
Use Georgia Medicaid’s online provider directory to locate in-network therapists. If you face access issues, contact Medicaid customer service for additional help. In areas with limited provider options, consider telehealth services, which Georgia Medicaid covers, as a flexible alternative.
Lack of coverage for certain treatments
Some types of therapy or alternative treatments, such as hypnotherapy or biofeedback, may not be covered by Georgia Medicaid.
What to try
Consult with your provider about alternative covered therapies. If you believe the denied treatment is medically necessary, you may file an appeal with supporting documentation from your provider explaining the necessity of the treatment for your condition.
By knowing how to navigate these common issues, you can better maintain access to the mental health services you need under Georgia Medicaid.
Making the most of your mental health coverage with Georgia Medicaid
Understanding your mental health benefits under Georgia Medicaid is essential for maintaining your overall wellness. Regularly reviewing your plan details and staying informed about any updates to your coverage can help you maximize your benefits and avoid disruptions in care.
Being proactive about your mental health is crucial. Seek help early when you need it, and don’t hesitate to advocate for yourself if you encounter challenges like denied claims or the need for pre-authorization. Knowing how to navigate these processes can ensure you maintain access to necessary care. Additionally, explore all available treatment options, including alternative and preventive care options such as wellness programs, group therapy, or telehealth services, to support your mental health comprehensively.

