Mental health care can be expensive, with therapy costs adding up quickly. For those covered by TennCare, Tennessee’s Medicaid program, there’s good news—your mental health care may be covered. This article breaks down what’s covered, what’s not, and how to navigate TennCare to get the mental health care you need.
Key takeaways
- TennCare, Tennessee’s Medicaid program, offers coverage for therapy, medication, and other behavioral health services to eligible residents.
- TennCare typically covers therapy types like CBT, DBT, family therapy, and substance use disorder treatment, both in-person and online. Some specialized therapies may require prior authorization.
- Many TennCare enrollees have little to no out-of-pocket costs for therapy, but co-pays may apply depending on the specific plan and income level.
- For certain therapies or medications, TennCare requires pre-approval, which involves documentation of medical necessity by a provider.
- You can contact TennCare or your Managed Care Organization (MCO) directly to confirm coverage, find providers, or resolve billing and authorization issues.
Introduction to TennCare
TennCare is Tennessee’s Medicaid program, offering health benefits to eligible low-income residents, including pregnant women, children, parents or caretakers of minor children, and individuals who are elderly or have disabilities. The program provides comprehensive coverage including medical, dental, and behavioral health care services for Tennessee residents.
TennCare’s mental health and behavioral health coverage includes a range of services, such as individual and group therapy, inpatient and outpatient treatment, crisis intervention, and substance use disorder services. These benefits aim to support Tennesseans in accessing the care they need for mental wellness and recovery.
Who is eligible for TennCare ?
TennCare provides health coverage to low-income individuals and families in Tennessee who meet specific eligibility criteria. To qualify, applicants must be Tennessee residents and meet income thresholds based on household size and specific circumstances, such as pregnancy, disability, or being the parent or caretaker of a minor child. Eligibility is also determined by resource limits, including the value of assets like cars and bank accounts.
Special groups, including children, pregnant women, and individuals with disabilities, receive tailored benefits under TennCare. For example, children are covered under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, which ensures access to comprehensive and preventive health services. Pregnant women may qualify for extended postpartum coverage, and those with disabilities can access specialized long-term care services.
To receive mental health services under TennCare, the therapy or treatment must be deemed “clinically necessary.” This determination is made by a qualified provider, based on whether the service is essential to prevent, diagnose, or treat a condition that significantly impairs daily functioning or poses a risk to the individual’s health. Coverage decisions are guided by TennCare’s policies and require providers to document the need for care.
Does TennCare cover therapy?
Yes, TennCare typically covers therapy — including in-person and online therapy — as well as a wide range of mental health services that are designed to help with substance abuse, trauma, depression, anxiety, stress, relationship issues, OCD and more.
What therapy does TennCare cover?
TennCare insurance covers many types of therapy for a wide variety of conditions. You will need to confirm what types of therapy your specific TennCare plan covers, but in general, the types of therapy TennCare typically covers includes:
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Applied behavior analysis (ABA) for Autism
- Substance use disorder treatment
- Inpatient and outpatient therapy
- Crisis intervention services
- Medication management
- Individual therapy
- Family therapy
- Group therapy
Other types of therapy that TennCare may cover, depending on diagnosis, previous therapies, and your TennCare plan details:
- Psychological testing
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation (TMS)
As some therapies require prior approval or additional documentation to establish medical necessity, it’s important to work closely with your TennCare provider to ensure coverage and explore all available options.
Learn more about other types of therapy you might find when seeking mental health care, and be sure to double check your specific TennCare health plan, or reach out to TennCare directly, to understand what therapy may be covered by your TennCare insurance.
Search for therapists who accept TennCare Medicaid
Medication coverage with TennCare
TennCare provides coverage for a wide range of psychiatric medications, ensuring that individuals with mental health conditions have access to treatments that support their recovery and well-being. Covered medications typically include:
- Antidepressants: Medications like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), commonly used to treat depression and anxiety disorders
- Antipsychotics: Drugs prescribed for conditions such as schizophrenia, schizoaffective disorder, or severe depression
- Mood stabilizers: Often used to manage bipolar disorder or mood dysregulation
- Anxiolytics: Medications to help with anxiety or panic disorders
- Stimulants and non-stimulants: For the treatment of ADHD and related conditions
Some high-cost or specialized medications may require prior authorization. This means your provider must submit documentation to TennCare’s pharmacy plan to demonstrate that the medication is medically necessary and appropriate for your condition. TennCare also maintains a Preferred Drug List (PDL) that identifies medications covered without the need for prior authorization.
If a prescribed medication is not on the PDL or exceeds TennCare’s pharmacy limits, your provider may request an exemption or explore alternative treatment options. It’s important to work closely with your healthcare provider and TennCare to ensure seamless access to the medications you need.
What types of therapy does TennCare not cover?
TennCare covers many types of therapy which may help an individual with their mental health needs. However, there are some types of mental health services which are not covered by TennCare. These services include, but may not be limited to:
- Therapies not deemed medically necessary
- Educational and developmental services
- Experimental or non-standard therapies
- Alternative or complementary therapies
- Private pay services
- Non-therapeutic counseling
- Hypnotherapy
- Non-traditional therapy such as biofeedback therapy
Does TennCare cover online therapy?
Yes, TennCare covers both online therapy (also referred to as telehealth or virtual therapy) as well as in-person therapy. Here are some important details about TennCare’s online therapy coverage:
- Provider requirements: Online therapy must be provided by a licensed therapist who is part of TennCare’s Managed Care Organization (MCO) network.
- Covered services: Virtual therapy can include individual, family, or group therapy, as well as medication management and other behavioral health services.
- Cost: Copays or coinsurance for online therapy are typically the same as for in-person visits, depending on your TennCare plan.
- Technology needs: Members will need access to a secure internet connection and a device capable of video conferencing.
- Prior authorization: Some services, such as intensive therapy or psychological testing, may require prior approval, whether delivered online or in person.
To confirm your eligibility and find providers offering online therapy, contact your MCO or visit their online provider directory.
Does TennCare cover out-of-network therapy?
To receive maximum benefit coverage, TennCare participants must use a network provider. TennCare may cover out of network therapists with preauthorization.
If you want to see an out-of-network mental healthcare provider with TennCare, it may cost much more than seeing an in-network provider. You may have to pay out of pocket, and you should check beforehand to see if you will be able to file for any kind of reimbursement from TennCare. If you have questions about out-of-network therapy coverage, please refer to your TennCare summary of benefits (SOB) as described below, or contact TennCare directly.
How to check if your TennCare plan covers therapy
There are two main ways to find out if your TennCare plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your TennCare “Summary of benefits”
On the summary of benefits (SOB), look for a row that references mental health, behavioral health, or substance abuse services, as well as “outpatient services” (because therapy is considered to be outpatient care).
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your TennCare plan covers these mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered,” then your TennCare plan does not cover mental health services such as therapy.
To learn more about how Summary of Benefits are structured, you can refer to this sample SOB from the Centers of Medicare & Medicaid Services website.
2. Contact TennCare directly
Contacting TennCare directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for TennCare, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the TennCare website to log into your account, and either chat or email an TennCare representative directly
How much does TennCare therapy cost?
Most TennCare enrollees have minimal or no out-of-pocket costs for therapy services or mental health treatment. Preventive care services, such as check-ups and screenings, are provided at no cost. For other services, co-payments may apply based on income levels and specific plan details:
- TennCare Medicaid for adults: Typically, only pharmacy co-pays are required; other services generally do not have co-pays.
- TennCare standard members with incomes at or above 100% of the Federal Poverty Level (FPL): Co-pays may apply for various services, including therapy.
Co-pay amounts can vary, and it’s important to consult your specific TennCare plan or contact TennCare to understand any costs associated with therapy services.
These are average ranges, however, so if you are insured by TennCare the cost of therapy will depend on your plan’s specific coverage—you should always confirm your out-of-pocket costs before your appointment.
TennCare therapy copay
When paying for therapy, your copay (or copayment) is an important cost you should know about.
The copay is a fixed amount you have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double check your copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to TennCare support directly.
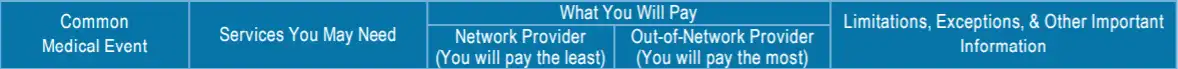
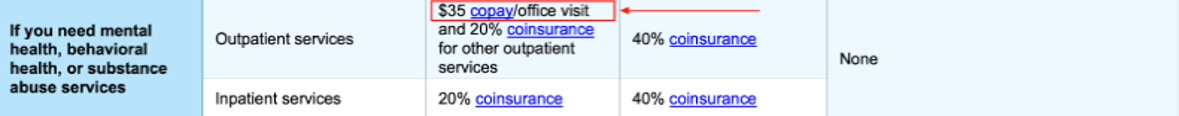
Sample image
What do terms like deductible, copay, and coinsurance mean?
Navigating the insurance system—especially when you’re in need of mental health support—can be challenging and confusing. For help, please visit our Understanding health insurance article.
Does TennCare require a referral to see a therapist?
Some plans may allow self-referral to in-network mental health providers, while others might require a referral from your primary care provider (PCP). To understand the referral policies applicable to your coverage, it’s essential to consult your MCO or review your member handbook. For more detailed information, visit the TennCare website.
How to find a therapist covered by TennCare
Finding a therapist who accepts TennCare insurance is not as difficult as you might think. To find a mental health professional covered by TennCare, you can contact TennCare customer service for assistance. They can help you locate in-network therapists and provide information about your mental health benefits.
TennCare Connect: Call toll-free at 855-259-0701 for assistance with applying for TennCare, reporting changes, or general information about your coverage.
For more information, visit the TennCare contact page.
Navigating common issues with TennCarehealth coverage
If you encounter challenges accessing mental health services through TennCare, this step-by-step guide can help you troubleshoot and resolve common issues.
Denied claims
A claim for mental health services is denied because TennCare determined the service was not covered, not medically necessary, or incorrectly filed.
What to try: Start by reviewing the explanation of benefits (EOB) or denial letter to understand the reason for the denial. Contact your TennCare Managed Care Organization (MCO) for clarification or to correct any billing errors. If you believe the denial was in error, file an appeal with TennCare, ensuring you include supporting documents from your provider that demonstrate the service’s necessity. For additional help, reach out to the TennCare Advocacy Program at 1-800-758-1638.
Needing pre-authorization
Certain mental health services, such as inpatient care, psychological testing, or intensive outpatient therapy, may require pre-authorization, and failing to obtain it can result in delays or denials.
What to try: Verify whether the service requires pre-authorization by reviewing your plan details or contacting your MCO. If authorization is needed, work with your provider to submit the necessary documentation. For services already rendered, ask your provider to request retroactive authorization. Be sure to follow up with your MCO to confirm approval before proceeding with treatment.
Provider availability issues
It can be challenging to find an in-network therapist, especially if there are long wait times or limited provider availability in your area.
What to try: Use your MCO’s online provider directory or call their member services for a list of in-network therapists. If you encounter difficulties, contact TennCare Connect at 855-259-0701 for further assistance. You might also consider virtual therapy, which many TennCare plans cover, as it can increase access and reduce wait times.
Incorrect billing
You may receive a bill for a service that should be covered under TennCare, often due to errors in coding or claim submission.
What to try: Review your TennCare member handbook or contact your MCO to confirm the service is covered. Then, reach out to your provider to verify that the claim was submitted correctly. If issues persist, dispute the charges by filing a complaint with TennCare or your MCO, providing documentation that supports your claim.
Lack of clarity on coverage
Uncertainty about whether a specific mental health service is covered can create delays in receiving care.
What to try: Contact your MCO to confirm whether the service is covered and whether pre-authorization is required. Review your TennCare member handbook or plan documentation for additional details. If possible, request written confirmation of coverage decisions for your records to avoid future disputes.
Whatever challenge that arises, by following these steps and utilizing available resources, you can resolve most issues and ensure you receive the mental health care you need through TennCare.
Making the most of your mental health coverage with TennCare
Understanding and utilizing your TennCare mental health benefits can make a significant difference in your overall well-being. By familiarizing yourself with what’s covered and staying informed about your plan details, you can access the care you need while avoiding unnecessary costs or delays.
Regularly review your TennCare coverage and stay updated on any changes to your benefits or requirements. Being proactive about your mental health—seeking help early, staying consistent with treatment, and addressing any challenges with your coverage—ensures you’re taking full advantage of the resources available to you.
Advocating for yourself is crucial. Don’t hesitate to reach out to your Managed Care Organization (MCO), TennCare customer service, or the TennCare Advocacy Program if you encounter obstacles. Additionally, explore alternative treatments and preventive care options to support comprehensive mental wellness. Whether through traditional therapy, medication management, or community-based support, TennCare offers tools to help you build a healthier future.

