Mental health care is a key part of overall well-being, but it can also be expensive, with the costs of therapy and treatment adding up quickly. If you’re covered by Ambetter insurance, you may have access to affordable mental health care services that can ease the financial burden. We’re here to help you understand how Ambetter can support your mental health needs, including what’s covered, what’s not, and how to use your coverage to get the care you need.
Key takeaways
- Ambetter insurance provides coverage for a range of mental health services including therapy, medication management, and specialized treatments.
- Costs for therapy with Ambetter vary by state and plan, with most sessions averaging $30–$50 after deductible and copay.
- Ambetter requires referrals for specialist visits, including therapy, and generally does not cover out-of-network providers.
- You can use Grow Therapy to find in-network therapists who accept Ambetter insurance and meet your specific needs.
What is Ambetter insurance?
Ambetter insurance offers health coverage through the Health Insurance Marketplace, with plans available in many states across the United States. Coverage options vary by state and individual needs, but most Ambetter plans include mental health services as part of their essential benefits.
Ambetter typically covers outpatient therapy, intensive outpatient programs, residential therapy, and medication management, all of which support mental health and substance abuse treatment. Whether you need one-on-one therapy or more intensive care, Ambetter can help you access services like cognitive behavioral therapy (CBT), family therapy, and group therapy.
What states is Ambetter available in?
Ambetter’s availability varies depending on the type of healthcare you’re looking for, including mental health services. Currently, Ambetter operates in 29 states. For mental health coverage through Grow Therapy, Ambetter therapists can be found in Florida, Indiana, Georgia, and Ohio.
Does Ambetter cover therapy?
Yes, Ambetter typically covers therapy—including in-person and online therapy—as well as a wide range of mental health services that are designed to help with substance abuse, depression, anxiety, stress, relationship issues, OCD, and more.
What therapy does Ambetter cover?
Ambetter insurance covers many types of therapy that serves as quality care options for many types of conditions. You need to confirm what types of therapy your specific Ambetter plan covers, but in general the types of therapy Ambetter typically covers includes:
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Eyemmovement desensitization and reprocessing (EMDR)
- Acceptance and commitment therapy (ACT)
- Exposure and response prevention therapy
- Internal family systems (IFS) therapy
Other types of therapy that Ambetter may cover, depending on diagnosis, previous therapies, and your Ambetter plan details:
- Addiction treatment
- Ketamine and esketamine (Spravato)
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation (TMS)
Ambetter covers mental health services from the following types of providers:
- Marriage and family therapists (MFT)
- Licensed clinical social workers (LCSW)
- Psychiatrists
- Nurse practitioners
- Licensed professional counselors
Learn more about other types of therapy you might find when seeking mental health care, and be sure to double check your specific Ambetter health plan, or reach out to Ambetter directly, to understand what therapy may be covered by your Ambetter insurance.
Search for therapists who accept Ambetter insurance
Medication coverage with Ambetter
Ambetter insurance typically covers a range of psychiatric medications used to treat mental health conditions such as depression, anxiety, ADHD, and mood disorders. Common medications covered may include antidepressants, antipsychotics, and mood stabilizers. However, for high-cost or specialized medications, such as certain brand-name drugs or newer treatments, prior authorization may be required. This means your healthcare provider must get approval from Ambetter before the medication will be covered to ensure it’s deemed medically necessary.
What types of therapy does Ambetter not cover?
Ambetter covers many types of therapy which may help an individual with their mental health needs. However, there are some types of mental health services which are not covered by Ambetter. These services include, but may not be limited to:
- Couples therapy: Because it is difficult to track a diagnosis when there is more than one person present, most health insurance plans do not cover couples therapy, Ambetter included.
- Hypnotherapy: Hypnotherapy uses hypnosis to help people with their mental health problems. Although some people find it helpful, Ambetter does not believe it is a reliable or effective treatment for mental health issues.
- Non-traditional therapy: Non-traditional therapy, such as biofeedback therapy, aims to help people control their body’s response to stress and anxiety by giving them feedback about their body’s functions, like their heart rate or blood pressure. Ambetter does not cover this type of therapy because they do not think there is enough evidence to prove that it’s an effective form of treatment.
Does Ambetter cover online therapy?
Yes, Ambetter covers both online therapy (also known as telehealth) and in-person therapy, offering flexible mental health care options. Online therapy through Ambetter is available in a number of states, including Alabama, Arizona, Florida, Georgia, Illinois, Indiana, Michigan, Texas, and Washington, among others. For consumers looking for online therapy through Grow Therapy with Ambetter coverage, this service is currently available in Florida, Indiana, and Ohio. Be sure to check your specific plan details to confirm availability in your state.
Does Ambetter cover out-of-network therapy?
Ambetter does not cover out-of-network services, except urgent care, emergency care or pre-approved services. To get the most out of your coverage with Ambetter, use the network that comes with your plan.
If you want to see an out-of-network mental healthcare provider with Ambetter, it may cost much more than seeing an in-network provider. You may have to pay out of pocket and file for reimbursement with Ambetter. If you have questions about out-of-network therapy coverage, please refer to your Ambetter summary of benefits (SOB) as described below, or contact Ambetter directly.
How to check if your Ambetter plan covers therapy
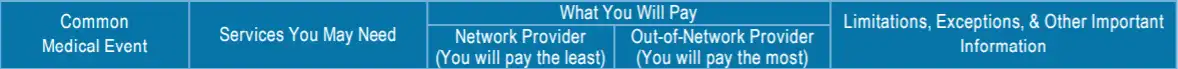
There are two main ways to find out if your Ambetter plan covers therapy and, if so, what it covers and how much it will cost.
1. Check your Ambetter “Summary of benefits”
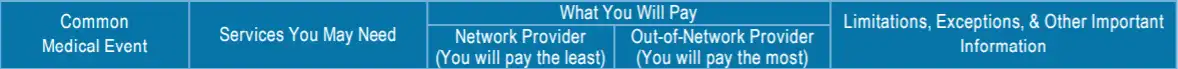
Sample image
If the “Network Provider” and/or “Out-of-Network Provider” give cost information, such as a copay or coinsurance, then your Ambetter plan does cover mental health services.
If the “Network Provider” and/or “Out-of-Network Provider” say “not covered”, then your Ambetter plan does not cover mental health services such as therapy.
To learn more about how summary of benefits are structured, you can refer to this sample SOB from Ambetter’s website.
2. Contact Ambetter directly
Contacting Ambetter directly is the best way to get the exact information you need about what types of mental health care are covered.
To find contact information for Ambetter, you can:
- Find the phone number to call, located on the back of your insurance ID card
- Use the Ambetter website to log into your account, and either chat or email an Ambetter representative directly.
How much does Ambetter therapy cost?
Most people who are insured by Ambetter will either be fully covered by their plan, or have to pay a small copay amount. For most clients, the average cost of Ambetter for therapy is $37.50 per session, after the deductible has been met.
- Florida – $30-$40
- Indiana – $40-$50
- Georgia – $30-$40
- Ohio – $30-$40
If you are insured by Ambetter the cost of therapy will depend on your plan’s specific coverage — you should always confirm your out-of-pocket costs before your appointment.
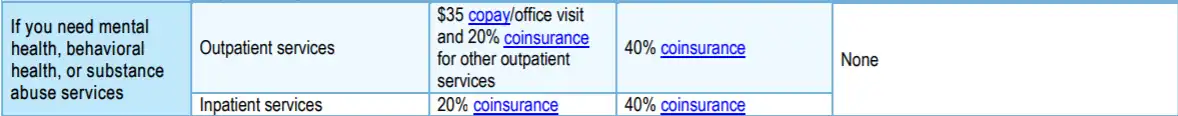
Ambetter therapy copay
When paying for therapy, your copay (or copayment) is an important cost you should know about.
The copay is a fixed amount you have to pay for each therapy session. Copays can vary depending on your plan, as well as the therapist you see, so it’s important to double check your copay under the mental health coverage section on your summary of benefits.
If you have any doubts or questions about if you have to pay a copay, or what your copay is, you should reach out to Ambetter support directly.
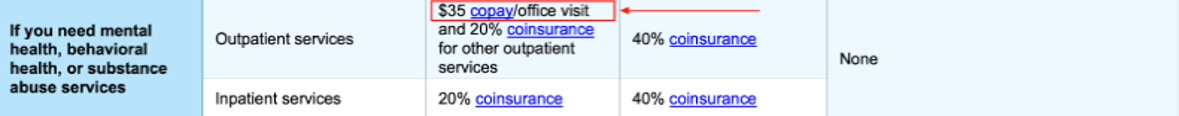
Sample image
Does Ambetter require a referral to see a therapist?
Ambetter generally requires a referral from your primary care physician (PCP) before you can see a specialist, including therapists for mental health services. You can easily confirm referrals through the Ambetter Virtual Access Member app. Without a referral from your PCP, your visit to a specialist will not be covered, and the claim will be denied. Be sure to check your plan and obtain the necessary referrals to avoid unexpected costs. For more details, visit the Ambetter website.
How to find a therapist covered by Ambetter
Finding a therapist who accepts Ambetter insurance is simpler than you might expect. There are a few ways to locate in-network providers:
1. Ambetter directory of therapists
Ambetter offers an online provider portal where you can search for mental health professionals. You can filter results by location, specialization, availability, and even check reviews, allowing you to find a therapist who meets your needs without having to call multiple offices.
2. Contact Ambetter customer service
If you prefer speaking to someone directly, you can contact Ambetter’s customer service for assistance to find a mental health provider who accepts your insurance. The phone number is on the back of your insurance ID card, or you can reach them via the Ambetter website.
3. Use Grow Therapy
With Grow Therapy, you can search for mental health providers who are in-network with Ambetter, who are licensed in your state and provide both online therapy or in-person therapy. On Grow Therapy, you can browse our growing network of vetted therapists and use filters to search by age, specialty, gender, and more. Simply pick the therapist who meets your unique needs and book your first session.
When booking, you’ll be asked to enter your insurance information to verify eligibility and receive a cost estimate.
Search Ambetter therapists by state:
What do terms like deductible, copays, and coinsurance mean?
Navigating the insurance system—especially when you’re in need of mental health support—can be challenging and confusing. For help, please visit our Understanding health insurance article.
Navigating common issues with Ambetterhealth coverage
Navigating issues with Ambetter health coverage for mental health services can sometimes be challenging. Here’s a guide to help you troubleshoot and resolve common problems:
Denied claims
If your claim for mental health services is denied, it could be due to a lack of proper documentation, missing referrals, or using an out-of-network provider.
Our solution: Review the denial notice carefully and gather all necessary documentation, such as medical records or referrals. You can appeal the decision by contacting Ambetter’s customer service or using their online portal to submit an appeal within the specified timeframe.
Needing pre-authorization
Some mental health services, especially high-cost or specialized treatments, may require pre-authorization. Without pre-approval, your claim could be denied.
Our solution: Before receiving treatment, confirm with your provider if pre-authorization is needed. Your provider can submit a request to Ambetter on your behalf. Always double-check that the authorization is in place before proceeding with the service.
Other common issues
Common problems might include confusion about in-network vs. out-of-network providers or coverage limits.
Our solution: Ensure that your therapist is in-network by using Ambetter’s provider directory or contacting customer service. Review your plan’s summary of benefits to understand any limits on the number of therapy sessions or services covered.
By staying informed and proactive, you can resolve issues quickly and avoid unexpected costs.
Making the most of your mental health coverage with Ambetter
Making the most of your mental health coverage with Ambetter starts with a clear understanding of your plan and the benefits available to you. Regularly reviewing your plan details ensures that you stay informed about any changes in coverage, helping you avoid surprises when seeking care. Being proactive about your mental health—seeking help early and advocating for yourself when challenges arise—can make a significant difference in your overall well-being.
Additionally, exploring alternative treatments and preventive care options, such as wellness visits and screenings, can contribute to comprehensive mental health care. By staying informed and taking advantage of your benefits, you can make meaningful strides toward better mental health with Ambetter’s support.

